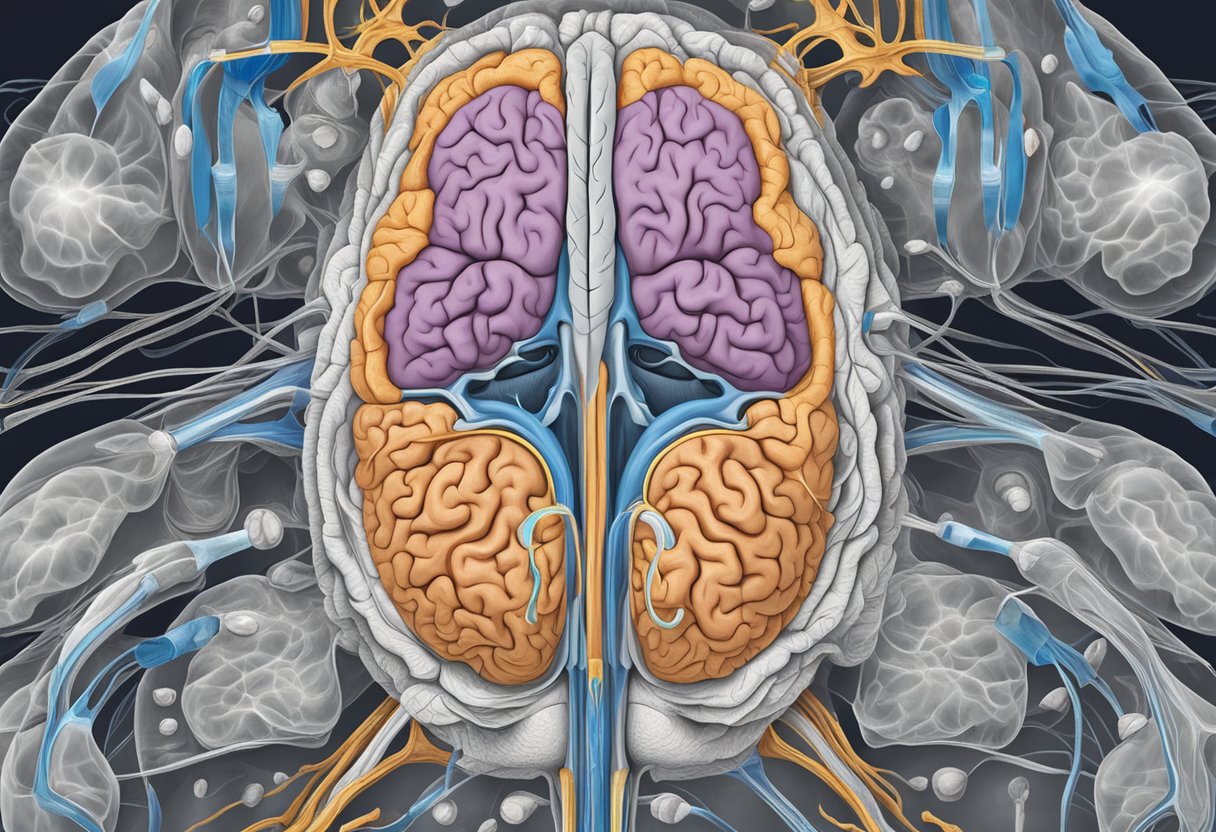
Bipolar disorder is a complex mental illness that significantly impacts various regions of the brain. The most affected areas include the prefrontal cortex and the hippocampus, which are crucial for decision-making, emotional regulation, and memory. Understanding how bipolar disorder alters brain structures is vital for effective treatment and management of the condition.
Studies indicate that individuals with bipolar disorder often experience thinning of the cortex in areas related to mood and cognition, particularly in the frontal and temporal regions. This structural change can contribute to the challenges faced in everyday functioning, influencing how you perceive and interact with the world around you. Recognizing these brain changes can pave the way for targeted therapy approaches.
If you or someone you know is navigating the complexities of bipolar disorder, it’s essential to seek support and professional guidance. Tides Mental Health offers comprehensive therapeutic options, including both virtual and in-person sessions, to help you manage the symptoms associated with this condition and improve your overall well-being.
Key Brain Regions Impacted by Bipolar Disorder
Bipolar disorder significantly affects various brain regions, leading to specific cognitive and emotional impairments. Understanding these areas can provide insight into the challenges faced by individuals with this condition.
Prefrontal Cortex
The prefrontal cortex plays a crucial role in planning, decision-making, and emotional regulation. In people with bipolar disorder, studies have shown abnormalities in the structure and function of this area.
Research indicates there may be reduced gray matter volume in the prefrontal cortex, impairing motivation and the ability to manage emotions effectively. This may manifest as impulsivity during manic episodes or indecision during depressive states. The prefrontal cortex’s involvement in higher cognitive functions highlights its importance in stabilizing mood and behavior.
Amygdala and Emotion Regulation
The amygdala is integral to processing emotions and is particularly sensitive to threats. In bipolar disorder, alterations in the amygdala can lead to heightened emotional responses.
Increased activation of the amygdala during emotional tasks has been documented, causing dysregulation in processing feelings such as happiness or sadness. This can result in intense mood swings and difficulties in controlling emotions. Understanding the amygdala’s role can help in identifying strategies for emotional regulation in therapy.
Hippocampus and Memory
The hippocampus is essential for memory formation and learning. Research has highlighted that individuals with bipolar disorder may experience structural changes in the hippocampus, affecting memory function.
These alterations often result in challenges with recalling information and learning new tasks. Emotional memories may also be particularly impacted, which can further complicate emotional stability. Addressing hippocampal function through therapeutic approaches could be vital in improving cognitive functioning in those affected.
Exploring these brain regions provides a foundation for understanding the complexities of bipolar disorder and potential pathways for effective treatment strategies.
Structural and Functional Brain Changes in Bipolar Disorder
Bipolar disorder is associated with significant changes in both the structural and functional aspects of the brain. These alterations can offer insights into the pathology of the disorder and help guide treatment approaches. Understanding these changes is crucial for developing effective strategies for management and therapy.
Grey Matter and White Matter Alterations
Research indicates that individuals with bipolar disorder experience reductions in both grey matter and white matter. The grey matter is critical for processing information, while the white matter facilitates communication between brain regions. Changes in these areas may lead to difficulties in mood regulation and cognitive function.
Studies have shown that the frontal lobe, limbic system, and other regions associated with emotional regulation may exhibit decreased grey matter volume. This could impair executive functions—such as planning and decision-making—which are often compromised in bipolar disorder.
Additionally, white matter abnormalities may affect the integrity of neural connections, influencing emotional responses and stability. These changes reflect the biological complexity of the disorder and emphasize the need for targeted therapeutic interventions.
Neuroimaging Findings
Neuroimaging techniques, particularly magnetic resonance imaging (MRI), have provided valuable insights into the brain’s structural changes in bipolar disorder. MRI studies frequently reveal alterations in specific brain regions, such as the prefrontal cortex and the hippocampus, both of which are crucial for mood regulation and emotional memory.
Research demonstrates that these imaging findings correlate with the severity of mood episodes. For instance, individuals experiencing manic episodes may exhibit accelerated cortical volume loss, while depressive states might be associated with structural deficits in limbic areas.
These neuroimaging outcomes can aid clinicians in identifying patterns associated with bipolar disorder. Furthermore, they may enhance understanding of the molecular psychiatry underlying the condition, promoting more personalized treatment approaches.
Neurobiological Mechanisms Affecting Brain Regions
Bipolar disorder involves complex neurobiological mechanisms that impact various brain regions. Key aspects include genetic factors and the role of neurotransmitters, both of which influence brain function and structure.
Gene Expression and Genetic Influences
Genetic predisposition plays a critical role in bipolar disorder. Studies indicate that family history significantly increases the likelihood of developing the condition. Specific genes associated with neurotransmission and mood regulation may exhibit altered expression in affected individuals.
Research has identified several candidate genes that may contribute to pathophysiology. Gene variants impacting the functioning of neurotransmitter systems, particularly serotonin and dopamine, are heavily studied. These alterations can affect neural connectivity within the prefrontal cortex and amygdala, regions crucial for mood regulation.
Key Points:
- Family history increases risk.
- Variants may alter neurotransmitter function.
Neurotransmitters and Molecular Pathways
Neurotransmitter systems significantly influence mood disorders. In bipolar disorder, dysregulation of catecholamines, particularly norepinephrine and dopamine, has been observed. These neurotransmitters impact regions responsible for emotional control and cognitive function.
Molecular pathways involving second messengers, such as cyclic AMP and phosphoinositides, also play a role. Abnormal signaling in these pathways can lead to disrupted mood regulation and cognitive impairments.
Important Areas:
- Prefrontal cortex: Decision-making and emotion.
- Amygdala: Emotional processing.
Understanding these mechanisms aids in recognizing how bipolar disorder manifests in individuals and highlights the importance of tailored therapeutic approaches. If you’re seeking support, Tides Mental Health offers resources for managing anxiety, depression, and life transitions effectively.
Impact of Bipolar Episodes on the Brain
Bipolar disorder significantly influences brain structure and function, particularly during episodes of mania and depression. These fluctuations can affect memory, cognitive processing, and emotional regulation, revealing distinct changes in brain activity.
Manic Episodes and Brain Activity
During manic episodes, heightened brain activity can lead to increased impulsivity and psychosis. Neuroimaging studies show that areas like the prefrontal cortex and amygdala exhibit abnormal activation. This may result in altered motivation and decision-making processes.
Key findings include:
- Increased Dopamine Activity: Elevated levels impacting workflow and goal-setting.
- Hyperactivity in the Amygdala: Enhances emotional responses and can lead to aggressive behavior.
As a result, individuals may struggle with self-control and experience challenges in social interactions, leading to potential conflicts.
Depressive Episodes and Cognitive Processing
In depressive episodes, brain abnormalities become more pronounced. Reduced activity in regions responsible for motivation and memory, such as the hippocampus, affects cognitive function. This often manifests as difficulty concentrating or remembering information.
Characteristics include:
- Decreased Prefrontal Cortex Activity: Impairs reasoning and emotional regulation.
- Memorial Impairments: Heightens forgetfulness, further lowering motivation levels.
Such changes can leave you feeling overwhelmed, affecting daily life and overall well-being. Addressing these episodes through therapy might help mitigate cognitive decline and facilitate healthier coping strategies. For those seeking support, Tides Mental Health offers solutions tailored to your needs.
Treatment Effects on Brain Structure and Function
Understanding how treatment can influence brain structure and function is critical for those managing bipolar disorder. Various medications play a significant role in mitigating symptoms and altering the brain’s physical properties.
Mood Stabilizers and Lithium
Mood stabilizers, particularly lithium, are foundational in treating bipolar disorder. Lithium treatment can lead to increased gray matter volume in specific brain regions. Research indicates that lithium may positively affect the medial temporal lobe and the limbic system.
These structures are vital for emotional regulation and memory processing. By enhancing these areas, lithium can help stabilize mood and reduce the frequency and severity of episodes. Regular monitoring is essential, as lithium levels must remain within a therapeutic range for safety and efficacy.
Antipsychotics and Antidepressants
Antipsychotics and antidepressants also influence brain function and structure. Antipsychotic medications can induce changes in dopamine transmission, which is crucial for mood regulation. These medications may help reduce psychotic symptoms, thus impacting areas like the prefrontal cortex.
Antidepressants target neurotransmitters, such as serotonin and norepinephrine, affecting mood and anxiety levels. Ongoing research shows that these medications can lead to structural changes, including increased cortical thickness in certain regions. This can result in improved cognitive function and emotional stability over time.
Ultimately, both mood stabilizers and other psychiatric medications play vital roles in shaping the brain’s architecture and function, contributing to effective management of bipolar disorder.
Advances in Research and Future Directions
Recent advances in bipolar disorder research have focused on understanding the brain’s structural and functional changes. Significant studies are shaping our knowledge of the neurological basis of this condition, while innovative technologies are enhancing research methodologies.
Leading Researchers and Landmark Studies
Ellen Leibenluft is among the leading researchers making strides in understanding bipolar disorder. Her work has emphasized the role of the amygdala and its connections to mood regulation. Landmark studies utilizing MRI have shown clear structural abnormalities in the brains of individuals with bipolar disorder.
For example, a neuroimaging study revealed that areas like the prefrontal cortex and hippocampus are notably affected. These findings indicate that bipolar disorder may disrupt neural pathways involved in emotional regulation. Ongoing research continues to explore these connections to develop more effective interventions.
Emerging Technologies in Brain Study
Emerging technologies like functional magnetic resonance imaging (fMRI) are revolutionizing the study of bipolar disorder. These technologies allow for real-time observation of brain activity patterns, providing insights into how different regions interact.
For instance, fMRI studies have illuminated the role of the limbic system, particularly the amygdala, in mood disorders. Researchers are applying advanced analytics to interpret complex data from neuroimaging, improving diagnostic accuracy.
As these methods evolve, there is potential for identifying early markers of bipolar disorder, paving the way for timely and targeted therapeutic options. Engaging with professionals knowledgeable in these advancements is crucial for those impacted by the disorder. Consider reaching out to Tides Mental Health for support and resources tailored to individual needs.
Frequently Asked Questions
Understanding the impact of bipolar disorder on the brain involves looking at various neurological factors, brain imaging, and neurotransmitter activity. This section addresses common questions regarding the specific brain areas affected and the implications for neurological functioning.
What are the neurological correlates of bipolar disorder?
Bipolar disorder is associated with alterations in brain structure and function. Key areas include the prefrontal cortex and hippocampus, which are involved in mood regulation and memory processing.
Can brain scans reveal indicators of bipolar disorder?
Yes, brain scans such as MRIs may show structural changes linked to bipolar disorder. These scans can highlight variations in gray matter volume and other morphological differences in the brain.
What role do neurotransmitters play in bipolar disorder?
Neurotransmitters are critical in regulating mood and behavior. Imbalances in substances like serotonin, dopamine, and norepinephrine are often observed in individuals with bipolar disorder, potentially influencing mood swings and other symptoms.
Does bipolar disorder lead to any form of brain damage?
There is evidence suggesting that chronic episodes of bipolar disorder may lead to structural brain changes. While this doesn’t equate to traditional brain damage, it can result in alterations that affect cognitive and emotional functioning.
What symptoms suggest brain impairment in bipolar disorder?
Symptoms such as impaired memory, difficulty concentrating, and reduced impulse control may indicate potential brain impairment. These issues can stem from changes in brain structure due to the disorder.
How does bipolar disorder affect neurological functioning?
Bipolar disorder can disrupt normal neurological functioning, leading to mood swings and challenges with attention and decision-making. These changes underscore the importance of addressing both mental health and neurological aspects through therapy. Consider reaching out to Tides Mental Health for support tailored to your specific needs.