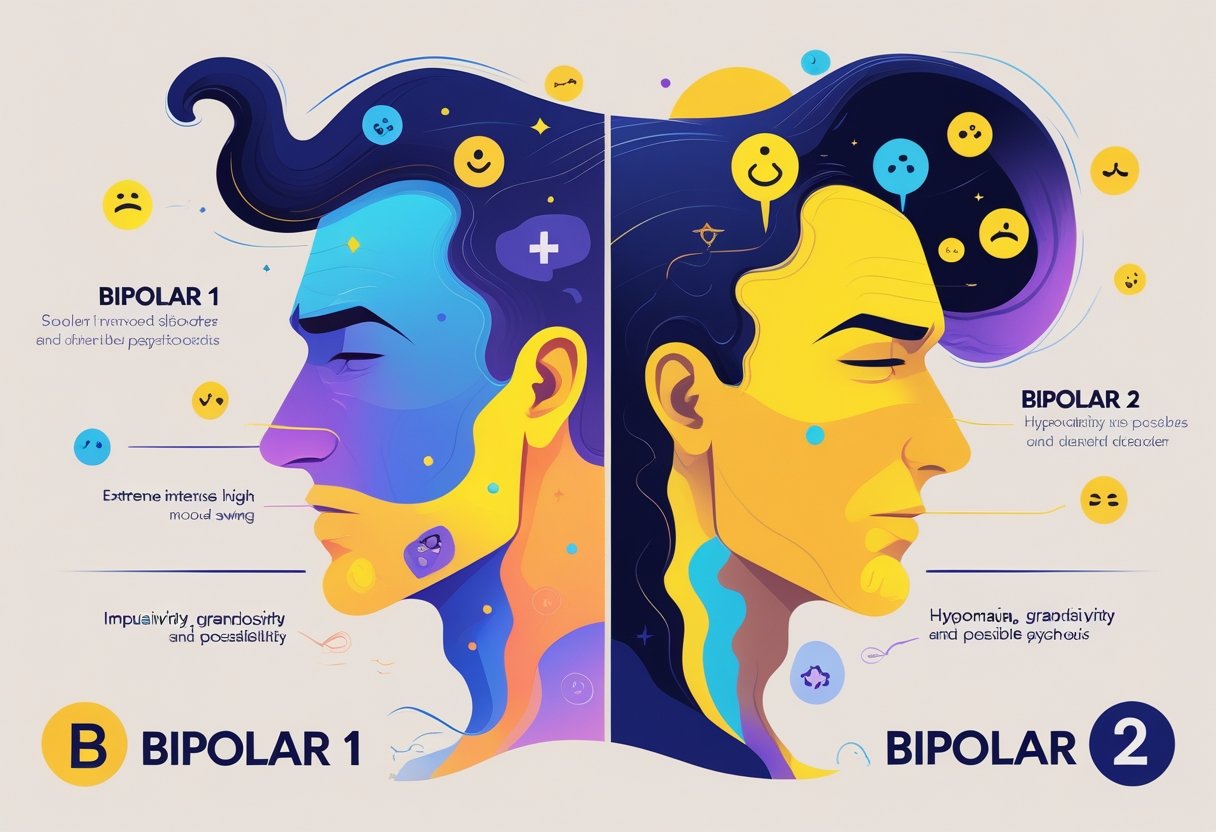
Understanding the differences between bipolar I and bipolar II disorders is crucial for anyone dealing with mood disorders or supporting someone who is. Bipolar I is characterized by severe manic episodes, while bipolar II includes hypomanic episodes and more frequent major depressive episodes. Recognizing these distinctions can guide effective treatment and improve your mental health journey.
Bipolar disorder significantly impacts mood, energy, and daily functioning. Knowing whether someone is experiencing the more intense conditions of bipolar I or the less severe manifestations in bipolar II can shape the approach to therapy and counseling. If you or someone you know is struggling, Tides Mental Health offers resources to help navigate these challenges, with options for both virtual and in-person sessions in the Chicago area.
As you read on, you’ll discover more about the symptoms, diagnosis, and treatment options for both types of bipolar disorder. This knowledge can empower you or your loved ones to seek appropriate support and live a more balanced life.
Core Differences Between Bipolar 1 and Bipolar 2
Bipolar 1 and Bipolar 2 disorders have distinct characteristics that influence diagnosis and treatment options. Understanding these differences is essential for effective management and support.
Manic Episodes in Bipolar 1
In Bipolar 1 disorder, a manic episode is a defining feature. This state typically lasts at least seven days and requires hospitalization, as it can present severe impairments in social or occupational functioning. During a manic episode, you may experience heightened energy, reduced need for sleep, grandiosity, and impulsiveness.
Symptoms can escalate to delusions or hallucinations, impacting your perception of reality. The intensity of these episodes distinguishes Bipolar 1 from Bipolar 2, where such severe manic episodes do not occur. Identifying and managing these manic episodes is crucial, as they can lead to significant consequences in daily life and relationships.
Hypomanic Episodes in Bipolar 2
With Bipolar 2 disorder, you experience hypomanic episodes that are less severe than the manic episodes seen in Bipolar 1. A hypomanic episode lasts for at least four consecutive days and is associated with noticeable changes in mood and activity levels. While you may feel unusually energetic and productive, these symptoms do not lead to the extreme dysfunction typically seen in full manic episodes.
You might find that hypomanic episodes can feel enjoyable or productive, but they can lead to problems in personal and professional settings if not managed effectively. It’s important to recognize these episodes to ensure appropriate treatment and support.
Depressive Episodes in Both Types
Both Bipolar 1 and Bipolar 2 involve depressive episodes, which can be debilitating. In Bipolar 1, you may experience major depressive episodes that can last for weeks or even months. Symptoms can include hopelessness, changes in appetite, difficulty concentrating, and feelings of worthlessness.
In Bipolar 2, depressive episodes also occur, typically lasting longer than hypomanic episodes. These can profoundly affect your quality of life and overall well-being. Recognizing and addressing depressive symptoms is essential for both types of bipolar disorder, as effective management strategies can vary significantly.
Diagnostic Criteria and DSM-5 Distinctions
The diagnostic criteria for Bipolar 1 and Bipolar 2 are outlined in the DSM-5. For Bipolar 1, the presence of at least one manic episode is essential for diagnosis. In contrast, Bipolar 2 is marked by the occurrence of at least one hypomanic episode and one major depressive episode, without ever having a full manic episode.
This differentiation is critical for treatment plans and understanding the course of each disorder. Accurate diagnosis can lead to better outcomes and appropriate therapeutic strategies tailored specifically to your needs. Engaging with mental health professionals who specialize in these disorders can provide valuable support and guidance. Tides Mental Health offers options for those seeking solutions, with sessions available both virtually and in person for individuals located in the Chicago area.
Unique Patterns and Symptom Severity
Understanding the unique patterns and symptoms associated with bipolar I and II disorders is crucial for recognizing the differences in mood cycling and severity. Each type presents distinct characteristics that can significantly impact your daily life and functioning.
Mood Cycling and Episode Duration
In bipolar I disorder, you experience more severe mood cycling, often alternating between intense manic episodes and depressive phases. Manic episodes typically last at least seven days and can be accompanied by a sense of euphoria and heightened energy levels. In contrast, bipolar II disorder features hypomanic episodes that are less severe, lasting a minimum of four consecutive days. The depressive episodes in bipolar II often last longer than those in bipolar I, sometimes extending for several weeks or months, which can complicate the diagnosis and treatment.
Mixed Episodes and Mood Swings
Mixed episodes are common in both bipolar disorders but are more frequently observed in bipolar I. You may find yourself experiencing feelings of both mania and depression simultaneously, leading to heightened emotional distress. Mood swings can be rapid and intense, often resulting in mood instability. This can manifest as irritability combined with energy surges or persistent sadness with racing thoughts. In bipolar II, mixed episodes can still occur, though they are typically less intense, often presenting with milder symptoms that make diagnosis more challenging.
Presence of Psychosis: Delusions and Hallucinations
Psychosis, characterized by delusions and hallucinations, is more commonly associated with bipolar I disorder. During severe manic episodes, you may encounter delusions of grandeur or experience auditory and visual hallucinations. These symptoms can significantly affect perception and reality, requiring immediate intervention. Bipolar II disorder can also present psychotic features, particularly during depressive episodes; however, this is less common. Awareness of these symptoms is vital, as they require distinct therapeutic approaches and potentially more intensive management for effective treatment.
Recognizing these unique patterns can help you navigate the complexities of bipolar disorders and inform your treatment options.
Diagnosis and Challenges in Identification
Identifying bipolar disorders can be complex due to overlapping symptoms and variations in presentation. Mental health professionals play a critical role in accurate diagnosis and addressing potential misdiagnosis. Understanding these challenges is vital for effective treatment.
Overlapping Symptoms
Bipolar I and II disorders share several symptoms, which can lead to confusion during diagnosis. Both types may involve episodes of depression, but the presence of mania distinguishes bipolar I from bipolar II, which features hypomania instead. Symptoms such as irritability, fatigue, and difficulty concentrating can occur in both disorders, complicating the assessment.
Moreover, these overlapping features may be mistaken for a major depressive episode or other mood disorders, including cyclothymic disorder. Mental health professionals must rely on comprehensive evaluations, including mood tracking, to differentiate between these conditions effectively. A thorough understanding of the distinct characteristics of each disorder is essential.
Misdiagnosis and Delayed Recognition
Misdiagnosis is a significant concern when identifying bipolar disorders. Many individuals may initially be diagnosed with unipolar depression, particularly if they present with primarily depressive symptoms. This oversight can lead to inappropriate treatment, such as prescribing antidepressants that may trigger manic episodes in bipolar patients.
Delayed recognition may also occur if mental health professionals do not thoroughly explore the patient’s mood history or previous episodes. A structured approach, including tools for mood tracking, can support accurate diagnosis by presenting a clearer picture of mood fluctuations over time. Awareness of these challenges can empower individuals and their families to advocate for proper assessments.
Role of Mental Health Professionals
Mental health professionals, particularly psychiatrists and clinical psychologists, play a vital role in diagnosing bipolar disorders. They utilize established diagnostic criteria from the DSM-5, which outlines specific symptoms and timeframes for mood episodes. Accurate diagnosis requires a comprehensive evaluation that considers medical history, family history, and current functioning.
Engagement in regular therapy sessions assists in ongoing assessment and adjustment of treatment plans. Professionals also educate patients about their disorders, helping them recognize early signs of mood changes. By fostering a collaborative relationship, mental health providers can significantly improve outcomes and ensure an accurate diagnosis, enabling you to receive appropriate care tailored to your needs. If you’re seeking support in navigating these challenges, Tides Mental Health offers services that cater to various age groups and preferences, including virtual and in-person options in the Chicago area.
Treatment Approaches for Bipolar 1 and Bipolar 2
Effective treatment approaches for Bipolar 1 and Bipolar 2 disorders focus on stabilizing mood and preventing episodes. These strategies include a combination of medications and psychotherapy tailored to individual needs.
Mood Stabilizers and Lithium Use
Mood stabilizers are essential in managing both Bipolar 1 and Bipolar 2 disorders. These medications help to balance mood swings and prevent manic or depressive episodes. Lithium is one of the most widely prescribed mood stabilizers. It has shown efficacy in reducing the frequency and severity of manic episodes.
You may find that lithium requires regular blood monitoring due to potential side effects. Other common mood stabilizers include valproate and lamotrigine, which may be prescribed based on your specific symptoms. Incorporating mood stabilizers into your treatment plan can significantly improve stability and quality of life.
Antipsychotics and Atypical Antipsychotics
Antipsychotics are often used alongside mood stabilizers, particularly for managing acute mania in Bipolar 1. Atypical antipsychotics like quetiapine and olanzapine are common choices. They can help reduce manic symptoms and provide stabilization during depressive phases.
These medications are particularly useful if mood stabilizers alone are not sufficient. They often come with side effects like weight gain or drowsiness, so monitoring is essential. Discussing these aspects with your healthcare provider can help ensure you find an effective balance in your treatment plan.
Antidepressants in Bipolar Depression
Antidepressants can be a point of contention in treating bipolar disorders. While they may alleviate symptoms of depression, they can also potentially trigger manic episodes, especially in Bipolar 1. Your clinician may prescribe them cautiously and typically in conjunction with mood stabilizers for safety.
Selective serotonin reuptake inhibitors (SSRIs) and bupropion are commonly explored options. It’s crucial to monitor your response and communicate any changes in mood to your healthcare team. Educating yourself about these risks and benefits will empower you to make informed decisions regarding your treatment.
Psychotherapy and Cognitive Behavioral Therapy
Psychotherapy is an integral part of a comprehensive treatment plan for both types of bipolar disorder. Cognitive Behavioral Therapy (CBT) is particularly effective, focusing on identifying and changing negative thought patterns.
CBT can help you develop coping strategies and improve your ability to manage mood episodes. It often addresses specific issues like anxiety, depression, and life transitions. Your therapist may guide you through setting achievable goals and learning skills to handle stress better. For those seeking professional support, Tides Mental Health offers accessible virtual and in-person psychotherapy options tailored to your needs.
Long-Term Management and Quality of Life
Long-term management of bipolar disorder significantly impacts your quality of life. Effective strategies can enhance stability, minimize symptoms, and encourage positive social interactions. Focusing on the following areas can help you build a supportive and healthy routine.
Psychoeducation and Support Strategies
Psychoeducation is crucial for individuals with bipolar disorder and their support networks. Understanding your condition empowers you to identify triggers and manage symptoms effectively. Engaging in therapy sessions that focus on education can help clarify the disorder’s nature, preventing misconceptions. Support strategies, including family involvement, enhance emotional backing and resilience.
Consider joining support groups where shared experiences can provide insight and coping techniques. Educational resources, whether articles or workshops, can foster a deeper understanding of personal challenges and how to address them. Engaging in continuous learning helps you adapt to changing circumstances and maintain a proactive approach.
Lifestyle Adjustments and Sleep Schedule
Lifestyle adjustments play a pivotal role in managing bipolar disorder. Establishing a consistent sleep schedule is essential, as disrupted sleep can trigger manic or depressive episodes. Aim for a regular bedtime and wake-up time to support your circadian rhythm, which can improve mood stability.
Incorporating healthy eating habits and regular exercise into your routine also contributes to overall well-being. Balanced nutrition can enhance mood and energy levels. Physical activity releases endorphins, which help reduce anxiety and depressive symptoms.
Making small, manageable changes to your daily routine can lead to significant improvements in your quality of life.
Interpersonal and Social Rhythm Therapy (IPSRT)
Interpersonal and Social Rhythm Therapy (IPSRT) is an evidence-based treatment designed to stabilize mood by focusing on relationships and regulating daily rhythms. This therapy encourages you to identify and improve interpersonal relationships while emphasizing the importance of daily routines.
By recognizing the connections between social interactions, mood, and regularity in daily life, IPSRT aims to enhance your emotional resilience. You learn to develop routines that align with your personal needs and life circumstances. Engaging in this type of therapy can result in a more balanced lifestyle, helping you navigate challenges effectively.
Monitoring Substance Abuse and Stress
Monitoring substance abuse is vital for those with bipolar disorder, as substance use can complicate management and exacerbate symptoms. Stay vigilant about your usage patterns, seeking help if you notice increased consumption of alcohol or drugs, which can lead to manic or depressive episodes.
Stress management techniques are equally important. Practices such as mindfulness, relaxation exercises, and regular physical activity can mitigate stress and directly influence your mood stability. Learn to recognize stressors in your life, and develop strategies to address them proactively. Building a network of support—friends, family, or professionals—can also provide the assistance you need during challenging times.
By addressing substance abuse and stress, you contribute to a more stable and fulfilling life.
Frequently Asked Questions
This section addresses common inquiries regarding the differences between Bipolar I and Bipolar II disorders. The focus will be on symptom distinctions, treatment approaches, diagnosis, prevalence rates, and episodes related to each disorder.
What are the distinguishing symptoms between Bipolar I and Bipolar II?
Bipolar I disorder is characterized by the presence of at least one manic episode, which can lead to significant impairment in daily functioning. In contrast, Bipolar II disorder involves hypomanic episodes that are generally less severe than full-blown mania but are often accompanied by major depressive episodes.
This key difference in the intensity and type of mood episodes is essential for accurate diagnosis and treatment.
How do the treatment options for Bipolar I differ from Bipolar II?
Treatment for Bipolar I often involves mood stabilizers and antipsychotic medications to manage manic episodes effectively. Therapy may also focus on crisis management due to the intensity of these episodes.
For Bipolar II, treatment typically emphasizes managing depressive symptoms, often using different combinations of antidepressants and mood stabilizers while monitoring for triggers of hypomania.
Can someone be diagnosed with both Bipolar I and Bipolar II disorder?
It is uncommon for a person to receive a dual diagnosis of both Bipolar I and Bipolar II. Generally, the presence of manic episodes suggests Bipolar I, while hypomanic and depressive episodes align more with Bipolar II. A comprehensive evaluation by a mental health professional is necessary for accurate diagnosis.
What is the prevalence rate of Bipolar I relative to Bipolar II?
Bipolar I disorder is estimated to occur in about 1% of the population, while Bipolar II disorder is more prevalent, affecting approximately 2-3% of individuals. These differences highlight the varying levels of severity and how they manifest in different individuals.
How are manic episodes in Bipolar I different from hypomanic episodes in Bipolar II?
Manic episodes in Bipolar I are marked by severe disruptions, including extreme energy, euphoria, and potential risk-taking behaviors. These episodes can lead to hospitalization due to their intensity.
In contrast, hypomanic episodes in Bipolar II are less severe and do not cause significant impairment, making it challenging to recognize without a detailed assessment of mood patterns.
What are the key differences between Cyclothymia and Bipolar II disorder?
Cyclothymia involves numerous periods of hypomanic symptoms and depressive symptoms lasting for at least two years, but these symptoms do not meet the criteria for a hypomanic or depressive episode.
Bipolar II, on the other hand, includes distinct major depressive episodes alongside hypomanic symptoms, indicating a more chronic and severe presentation. Understanding these distinctions can aid in effective treatment strategies for each condition.