Shorter days and weaker sunlight can change how your brain works. Lower light disrupts your body clock, reduces serotonin, and raises melatonin, which can make you feel tired, low, and less motivated during certain seasons.
You might notice symptoms start in fall and peak in winter, or less commonly in summer. This post will explain the biology behind those changes, the role of genetics and hormones, and simple steps you can take now—including how Tides Mental Health can help with therapy options both virtually and in-person in the Chicago area.
What Is Seasonal Affective Disorder?
Seasonal affective disorder (SAD) is a type of depression that comes and goes with the seasons. It usually starts at the same time each year and affects your mood, sleep, energy, and daily routine.
Definition and Overview
Seasonal affective disorder is a pattern of major depressive episodes that repeat at a particular time each year. Most people experience SAD in late fall or winter, though a smaller number have symptoms in spring or summer.
The condition links to changes in daylight, which can disrupt your circadian rhythm and brain chemicals like serotonin and melatonin. Symptoms can include low mood, loss of interest in activities, changes in sleep or appetite, low energy, and trouble concentrating.
Healthcare providers diagnose SAD when depressive episodes follow a clear seasonal pattern for at least two years. Treatments often combine light therapy, counseling, and medication when needed.
Prevalence and Risk Groups
SAD affects a minority of people, but rates rise at higher latitudes where winter days are shorter. Women report SAD more often than men.
You face higher risk if you have a family history of depression or if you already have mood disorders like major depression or bipolar disorder. Other risk factors include less time spent outdoors and working or living in places with low winter sunlight.
If you need care, Tides Mental Health offers therapy focused on anxiety, depression, and life transitions, with most sessions available virtually and in-person options in the Chicago area.
Seasonal Patterns and Symptoms
Most people with SAD see symptoms begin in late fall and ease in spring. You might sleep more than usual, crave carbohydrates and gain weight, or feel sluggish and withdrawn.
Less common is summer-pattern SAD, which can bring insomnia, poor appetite, and agitation. Watch for severe signs such as thoughts of self-harm or an inability to function at work or home.
If symptoms match a seasonal pattern and impair daily life, seek assessment. Tides Mental Health provides targeted counseling and coping strategies to help reset routines, improve sleep, and manage seasonal mood changes.
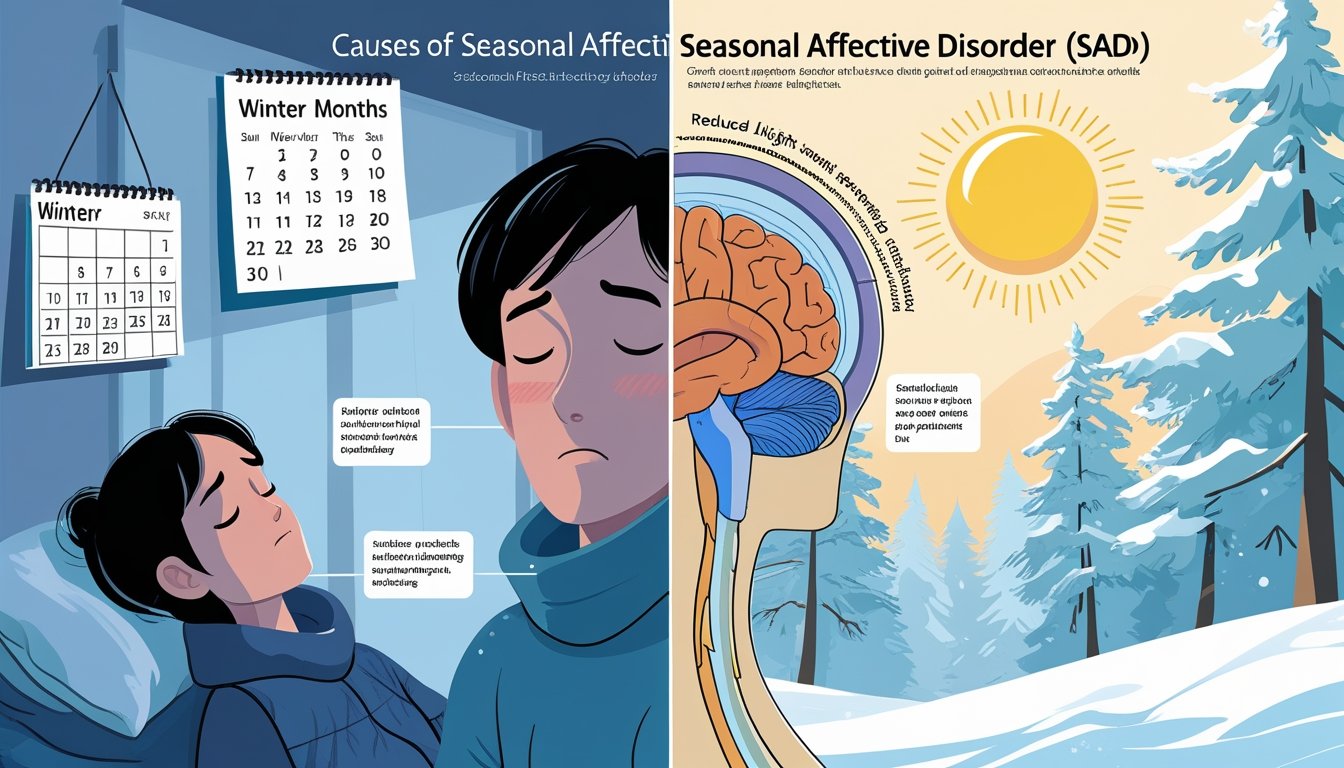
Biological Causes of Seasonal Affective Disorder
Biological factors link shorter daylight, shifts in daily rhythms, and brain chemistry changes to the seasonal pattern of symptoms. These body-based changes affect sleep, mood, energy, and appetite in predictable ways.
Role of Sunlight Exposure
Sunlight controls signals to your brain that regulate alertness and mood. Less daylight in fall and winter lowers the amount of light reaching your eyes.
That reduces stimulation of the retinal pathways that communicate with mood centers in the brain. Lower light also means less activation of the suprachiasmatic nucleus (SCN), the brain’s main clock.
When the SCN gets weaker light cues, it sends altered timing signals to hormones and sleep systems. That can leave you sleepy during the day, awake at night, or more irritable.
If you live at higher latitudes or spend long hours indoors, you face bigger drops in light exposure. Light therapy and increased outdoor time are common ways to restore those signals.
Changes in Circadian Rhythm
Your circadian rhythm times sleep, appetite, and hormone release over 24 hours. Shorter days can shift that rhythm later or make it less consistent.
When timing shifts, you may fall asleep later, wake feeling unrefreshed, or struggle to maintain regular routines. Disrupted circadian timing affects core body temperature, cortisol release, and sleep architecture.
These changes reduce daytime energy and worsen concentration. People with existing mood vulnerabilities feel these effects more strongly.
Regular sleep-wake times, morning light exposure, and structured daily activities help re-align your rhythm. If symptoms persist, therapy and targeted behavioral plans can support lasting schedule changes.
Melatonin Production
Melatonin is the sleep-related hormone your brain produces in darkness. Longer nights increase melatonin secretion and can prolong sleepiness into daytime hours.
In SAD, melatonin levels may stay higher at times when you need alertness. Abnormal melatonin timing causes grogginess, low motivation, and carbohydrate cravings.
People sensitive to melatonin shifts notice stronger seasonal fatigue and social withdrawal. You can reduce excess melatonin by getting bright light soon after waking, keeping evening light low, and avoiding late-night screens.
For some people, clinicians consider melatonin-timing strategies or light therapy under professional guidance.
Serotonin Levels
Serotonin helps regulate mood, appetite, and impulse control. Reduced sunlight lowers serotonin transporter activity and can reduce available serotonin in the brain.
That change links directly to increased sadness, carbohydrate cravings, and slowed thinking in winter months. Genetic differences in serotonin systems make some people more prone to this drop.
Low serotonin also interacts with circadian and melatonin changes, amplifying mood symptoms. You can address serotonin-related symptoms with behavioral changes, light therapy, and evidence-based therapy for depression and anxiety.
If symptoms are severe, discuss medication options and combined care with a provider. Tides Mental Health offers virtual and in-person counseling in the Chicago area to help you develop treatment plans focused on these biological factors.
Environmental and Lifestyle Factors
Sunlight, daily routines, and where you live can change your sleep, mood, and energy. Small shifts in light exposure and habits often make a big difference in how you feel each day.
Geographic Location and Climate
Where you live affects how much natural light you get each day. If you live far north or south, winter days can be short and dim.
Reduced daylight can shift your circadian rhythm and lower serotonin, which can cause low mood and tiredness. Cloudy, overcast climates also limit bright light even when day length is average.
Urban areas with tall buildings and small windows further reduce your direct sun exposure. If you notice mood shifts tied to seasons, consider tracking daylight hours and symptoms to spot patterns.
Tides Mental Health offers virtual options if you live far from Chicago or can’t travel. For in-person care, our Chicago clinic can help you make a plan that matches your local climate and light needs.
Daily Habits and Indoor Living
How you spend your day changes your light exposure and activity level. Long indoor work hours, small windows, and late bedtimes reduce daytime brightness and fragment sleep.
Less movement and more screen time at night can also blunt mood regulation. You can change simple habits: sit by the brightest window for morning tasks, get 20–30 minutes of outdoor light daily, and keep a regular wake time.
Use bright overhead lights or light boxes if natural light is limited. Keep evening screens dim and avoid caffeine late in the day to support sleep.
If habit changes feel hard, talk with Tides Mental Health. We provide therapy focused on depression, anxiety, and life transitions and can help you build daily routines that improve mood.
Work and Social Schedules
Your work hours and social life shape light exposure and stress. Night shifts, early morning commutes in the dark, or long indoor meetings cut into daylight and disrupt sleep cycles.
Irregular schedules also make consistent meals, exercise, and social contact harder to keep up. Social withdrawal in winter reduces rewarding activities and support.
Try scheduling regular social time, even brief video calls or walks with a friend. If work shifts force night hours, use timed bright light in the morning and blackout curtains for daytime sleep.
Tides Mental Health supports adults with flexible virtual sessions (60–70% remote) to fit varied schedules. Our Chicago in-person option can also help you adjust work and social routines to protect your mood.
Genetic and Personal Risk Factors
Genes and your past health shape how likely you are to get seasonal mood changes. Some people inherit traits that make their brain chemistry react to light shifts.
Your medical history and current health conditions also change your risk and the best steps to take.
Family History of Mood Disorders
If close relatives have depression, bipolar disorder, or SAD, your chance of developing seasonal depression rises. Studies show multiple genes likely add to risk rather than one single cause.
That means a family pattern of mood problems matters more than one isolated diagnosis. Genetic risk can affect how your brain handles serotonin and melatonin, the chemicals tied to mood and sleep.
Families who live far from the equator often show stronger patterns because larger seasonal light shifts interact with inherited sensitivity. Knowing family history helps you and your clinician choose treatments early.
You may respond better to light therapy or a combined plan of therapy and medication if relatives needed similar care.
Personal Health History
Your own past mental health events change risk. If you have had major depression, anxiety disorders, or bipolar disorder, you are more likely to develop SAD in seasons with reduced daylight.
Prior episodes also help predict how severe future seasonal symptoms could be. Physical health matters too.
Sleep problems, thyroid issues, and chronic medical conditions can worsen seasonal mood changes. Lifestyle factors — low outdoor time, working long indoor hours, and eye-level light exposure — increase risk because they lower daily light input.
When you seek help, Tides Mental Health offers therapy focused on depression and anxiety, with most sessions available virtually and in-person care in the Chicago area. Your provider will look at your personal and family history to build a clear treatment plan that fits your needs.
Impact of Hormones on Seasonal Affective Disorder
Hormones can change how your mood, sleep, and energy respond to shorter days. These shifts often affect two key systems tied to sleep and mood, which can make seasonal mood changes worse.
Hormonal Fluctuations in Winter
Shorter daylight raises melatonin for many people. Higher melatonin can make you feel sleepy, lower energy, and slow your daily rhythm.
Reduced sunlight can also lower serotonin activity. That change can make you more prone to low mood, irritability, and sugar cravings.
Women may notice stronger effects around menstrual changes or during perimenopause when estrogen levels shift. Men can also feel changes when testosterone drops with age or stress.
You can track sleep, appetite, and mood to spot patterns. If these symptoms start each fall or winter, mention them when you seek care.
Endocrine System Disruptions
The endocrine system links the brain and body through hormones. Light exposure affects the hypothalamus, which then alters melatonin from the pineal gland and influences cortisol from the adrenal glands.
Disrupted cortisol patterns can make stress harder to manage and worsen anxiety or low mood. Thyroid function also matters; low thyroid hormone can cause fatigue and depression that overlap with SAD.
Blood tests can check thyroid, cortisol, and sex hormones to rule out other causes. If you want help, Tides Mental Health offers adult therapy focused on depression, anxiety, life transitions, and couples or family work.
You can choose virtual sessions (60–70% of care) or in-person visits in the Chicago area (30–40%).
Other Contributing Factors
Reduced daylight is not the only thing that can raise your risk for seasonal depression. Two important causes are low vitamin D and other mental health conditions that interact with seasonal changes.
Both can make symptoms start earlier, feel worse, or last longer.
Vitamin D Deficiency
Low vitamin D can affect mood and energy because it helps regulate brain chemicals tied to depression. You can become deficient when you spend most of the day indoors, live at higher latitudes, or avoid sun exposure in fall and winter.
A blood test (25‑hydroxyvitamin D) shows if your level is low. If your levels are low, your doctor may recommend supplements or dietary changes.
Foods with vitamin D include fortified milk, fatty fish, and eggs, but supplements are often needed in winter. Tides Mental Health can help you decide on testing and treatment during a virtual or in‑person visit in the Chicago area.
Coexisting Mental Health Disorders
Having anxiety or nonseasonal depression raises the chance that seasonal changes will trigger worse symptoms. If you already struggle with panic, generalized anxiety, or major depressive disorder, shorter days can amplify sleep problems, rumination, and avoidance behaviors.
Treatment often combines therapy and medication. Cognitive-behavioral therapy helps with negative thinking and routine building.
If you work with Tides Mental Health, you can get therapy focused on anxiety, depression, life transitions, or family issues. Most sessions are virtual (60–70%), with in‑person care available in Chicago (30–40%) when you prefer face‑to‑face support.
Conclusion
Seasonal changes can shift your sleep, mood, and energy. Shorter days and less light often alter brain chemicals and your internal clock.
This can make you feel low during fall and winter. Light therapy, regular activity, and steady sleep schedules reduce symptoms for many people.
Medication and talk therapy also help when symptoms are more severe. If you want help that fits your life, Tides Mental Health offers therapy focused on depression, anxiety, life changes, and relationship issues.
You can choose virtual sessions for most care or in-person visits in the Chicago area. Therapists can work with adults now and plans exist to expand services for children and teens.
Watch for signs that need faster care, such as severe sadness, trouble functioning, or thoughts of harming yourself. Reach out to a clinician or emergency services right away if that happens.