You’ll find that an Intensive Outpatient Program (IOP) gives you structured, flexible care that fits around work, family, and daily life while treating anxiety, depression, relationship issues, and life transitions.\ An IOP combines regular therapy sessions, group work, and skill-building with a coordinated team so you get focused treatment without staying overnight.
This article will walk you through how IOPs are organized, what each team member does, the usual therapy and support services offered, and how programs link with other care levels.\ If you want options that include virtual care and in-person support in Chicago, Tides Mental Health can help you explore the right IOP format for your needs.
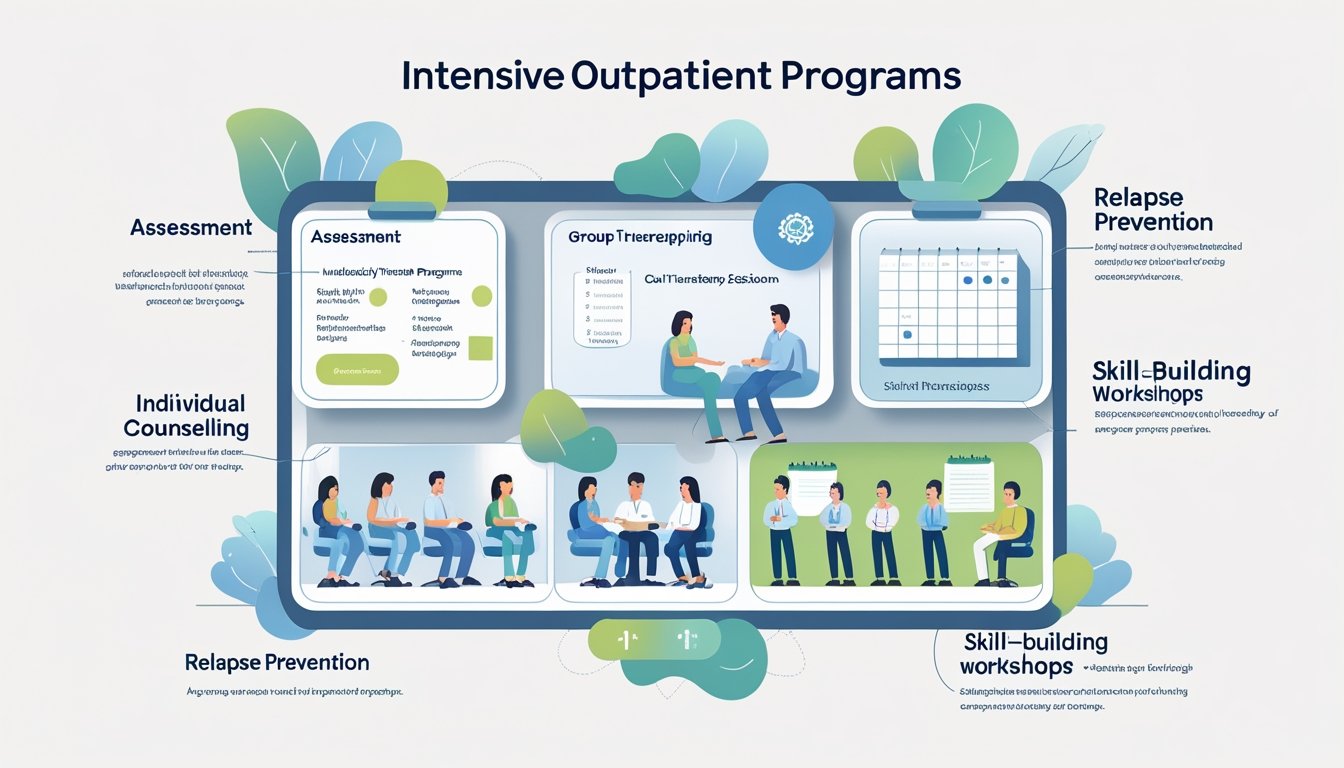
Overview of Intensive Outpatient Programs
IOPs give structured therapy without requiring you to live at the clinic.They combine regular therapy sessions, personalized treatment plans, and flexible scheduling so you can keep work, family, or school commitments.
Definition and Purpose
An intensive outpatient program (IOP) is a non-residential treatment option that provides frequent, scheduled therapy while you continue living at home.\ IOPs treat anxiety, depression, substance use, and life transitions through group therapy, individual counseling, and skill-building workshops.
You attend sessions multiple days per week for several hours each day, which creates a steady support routine without full hospitalization.\ Many participants move to IOP after inpatient care or use it instead of more intensive levels of care when detox is not required.
Tides Mental Health offers IOP services that are mainly virtual with in-person options in the Chicago area.
Key Features of IOPs
IOPs use a combination of approaches to meet your needs.\ Expect weekly individual therapy, group sessions focused on coping skills, and family or couples counseling when needed.
Treatment plans are personalized and reviewed regularly to track progress and adjust goals.\ Programs often include psychoeducation, relapse prevention, and medication management by licensed clinicians.
Scheduling typically runs several days per week with flexible evening or daytime slots to fit work or school.\ At Tides Mental Health, about 60–70% of sessions are virtual and 30–40% are in-person, which helps maintain continuity while letting you access care from home.
Benefits of Intensive Outpatient Programs
IOPs balance intensity with daily life so you keep your routines while receiving strong clinical support.\ You build coping skills in group settings, practice them between sessions, and get individual guidance on applying strategies to real-life situations.
This structure helps reduce symptoms of anxiety and depression, improve relationships, and ease major life transitions.\ If you need more support than weekly therapy but don’t require hospitalization, an IOP can prevent relapse and reduce the need for emergency care.
Tides Mental Health provides tailored IOP plans that focus on adult therapy and expanding services for children and adolescents.
Core Components of IOP Structure
The program combines one-on-one therapy, group work, and regular clinical review.\ It balances virtual care with in-person options in Chicago and centers treatment on anxiety, depression, life transitions, and couples/family needs.
Therapy Modalities Offered
IOPs use several evidence-based therapies tailored to adult needs.\ You will typically receive individual therapy for personalized goals and diagnosis-based treatment.
Expect Cognitive Behavioral Therapy (CBT) for anxiety and depression, Dialectical Behavior Therapy (DBT) skills for emotion regulation, and family or couples sessions to address relationships and communication.\ Group therapy complements individual work.
Groups focus on coping skills, relapse prevention, and role-play for interpersonal issues.\ Psychoeducation sessions teach symptom management and self-care routines.
Most sessions happen virtually (about 60–70%), with 30–40% in-person options in the Chicago area.\ Tides Mental Health is available if you want an organized program that blends virtual and face-to-face care.
Program Scheduling and Duration
An IOP typically runs 9–20 hours per week split into multiple sessions.\ You might attend three to five days weekly, with a mix of group and individual appointments.
Daily blocks often last 2–4 hours, allowing you to keep work or school responsibilities.\ Programs commonly run 8–12 weeks but can be shorter or extend based on progress.
Weekly schedules include fixed group times plus flexible individual therapy slots.\ Telehealth slots increase accessibility for those balancing family or job duties.
Tides Mental Health offers schedules that prioritize continuity: consistent group times with adaptable individual sessions, and the option to shift to more in-person care when needed.
Patient Assessment and Admission Criteria
You undergo a clinical intake that reviews symptoms, medical history, and current stressors.\ The assessment uses standardized screening tools for anxiety and depression and evaluates safety risks like suicidal thoughts or substance misuse.
Your insurance and ability to commit to the weekly hours also factor into admission decisions.\ IOPs accept adults with moderate symptoms who do not need 24-hour medical monitoring.
You may be referred to inpatient care if you require medical detox, constant supervision, or intensive medical treatment.\ Tides Mental Health screens each applicant and creates a personalized treatment plan when you qualify.
Multidisciplinary Team Roles
The team mixes clinical oversight, therapists, and support staff to deliver coordinated care for adults with anxiety, depression, life transitions, and couples/family issues.\ You’ll see clear role boundaries, shared treatment goals, and routine communication to keep each patient’s plan consistent across virtual and in-person care.
Clinical Leadership
Clinical leaders set the program’s clinical standards and supervise direct care.\ They include a medical director or clinical director who reviews intake assessments, approves treatment plans, and ensures medication management follows best practices when needed.
If you need medication evaluation, the clinical leader coordinates with prescribing providers and documents changes in the record.\ Leaders run weekly case review meetings to track outcomes and adjust care.
They monitor quality metrics like symptom reduction, attendance, and safety events.\ In your program, leaders also guide the expansion into child and adolescent services and ensure staff training for those new populations.
Therapists and Counselors
Therapists deliver the core treatments: individual CBT for anxiety and depression, couples and family counseling, and modules for life-transition skills.\ You’ll work with licensed clinicians who conduct structured sessions, assign homework, and track symptom scales each month.
Most sessions occur virtually (60–70%), but in-person options are available in the Chicago area when you prefer face-to-face care.\ Counselors coordinate care across modalities.
They document progress notes, share treatment goals on the care plan, and participate in multidisciplinary case reviews.\ If you move to child or adolescent services, therapists will adapt session length and involve caregivers as needed.
Support Staff Responsibilities
Support staff keep the program running smoothly so clinicians can focus on care.\ Care coordinators schedule sessions, handle referrals, and connect you to ancillary services like psychiatry, nutrition, or community supports.
They also guide you through insurance questions and consent forms.\ Administrative staff manage intake paperwork, maintain the electronic record, and send reminders to reduce missed appointments.
Technical support helps with virtual-session setup and troubleshooting.\ You can ask support staff to arrange in-person visits at the Chicago clinic or help you access Tides Mental Health for an integrated option.
Treatment and Support Services
You will find structured group work, one-on-one counseling, family involvement, and medication oversight designed to fit your life and clinical needs.\ Each service aims to help you manage anxiety, depression, life changes, or relationship issues while letting you keep work, school, and home routines.
Group Therapy Sessions
Group sessions meet on set days and focus on skills you can use right away.\ Typical groups run 60–90 minutes and cover topics like cognitive behavioral techniques for anxiety, behavioral activation for depression, relapse prevention, and communication skills for couples.
You join a small cohort of adults, often mixed ages, so you get peer feedback and practice new behaviors in a safe setting.\ Most groups meet virtually, reflecting our 60–70% telehealth model, but we also offer in-person groups in the Chicago area.
Groups follow a clear agenda: check-in, skill teaching, role-play or practice, and a brief check-out.\ Expect homework to reinforce what you learn between sessions.
Individual Counseling
Your one-on-one sessions target the specific problems you bring, such as panic attacks, persistent low mood, or stress from work or family change.\ Clinicians use evidence-based methods—CBT for anxiety and depression, interpersonal therapy for relationship and life-transition issues, and solution-focused techniques for concrete goal-setting.
You can choose virtual or in-person appointments, with most clients opting for telehealth for convenience.\ Sessions last 45–60 minutes and include assessment, treatment planning, skill practice, and progress reviews.
Your clinician adjusts frequency as you improve, from multiple weekly contacts to monthly check-ins.
Family Involvement
Family and couples work address patterns that keep problems active.\ Sessions teach communication, boundary-setting, and problem-solving.
You and your partner or family members learn specific tools, like structured problem solving and short behavioral experiments, to change interactions at home.\ We schedule family sessions around your availability and offer both virtual and Chicago-area in-person options.
Clinicians balance individual goals with family goals to make treatment relevant to daily life.\ When appropriate, therapists use brief psychoeducation so everyone understands diagnoses, medication effects, and relapse signs.
Medication Management
If medication can help your symptoms, a prescriber evaluates you and discusses options such as SSRIs for depression and anxiety or targeted medications for sleep and agitation.\ Medication visits focus on symptom tracking, side-effect checks, and dose adjustments.
Your safety guides all decisions; clinicians monitor response closely during early weeks.\ You can have medication visits virtually or in person.
Pharmacologic care pairs with therapy rather than replaces it.\ Your provider explains risks and benefits, coordinates with your therapist, and schedules follow-ups to make sure the medication supports your therapy goals.
Tides Mental Health provides these services and can be your point of contact for intake, scheduling, and coordinating virtual or Chicago-based in-person care.
Typical Patient Pathways in IOPs
You will move through clear steps that assess needs, set goals, and track progress.\ Expect an intake that collects history, a tailored plan that matches your life and goals, and ongoing checks to adjust care.
Intake and Orientation Process
When you first join, intake gathers medical history, substance use or mental health history, current medications, and risk factors.\ Expect structured forms and a clinical interview that usually lasts 60–90 minutes.
The team will screen for depression, anxiety, trauma, and any safety concerns.\ If you have suicidal thoughts or active withdrawal symptoms, staff will arrange urgent care or higher-level services.
Orientation explains schedule, attendance rules, privacy practices, and how virtual and in-person sessions work.\ Most programs offer a mix of sessions; currently about 60–70% are virtual and 30–40% are in-person, with in-person options based in the Chicago area.
You’ll learn how to join telehealth groups, use any platform, and who to contact for emergencies.
Customized Treatment Planning
Your clinician will use intake data to build a written plan with specific, measurable goals—examples include reducing panic attacks to X per week or staying sober for Y days.\ Plans combine individual therapy, group skills sessions, family or couples counseling, and medication management when needed.
Sessions focus on anxiety, depression, life transitions, and relationship work.\ If you attend virtually, therapists adapt exercises for remote use and send materials by secure portal.
Frequency is typically 9–19 hours per week, scheduled around your work or home life.\ Your plan will note expected duration (weeks to months), homework assignments, and criteria for stepping down care or moving to a higher level if needed.
Progress Monitoring
Staff track progress with regular symptom scales, session attendance, and behavior-based goals.\ You’ll complete brief measures (for example, PHQ-9 or GAD-7) every 1–2 weeks and review results with your clinician.
Therapists hold case reviews to discuss improvements, setbacks, and any medication response.\ If you miss sessions or show risk signs, the team adjusts intensity or adds family sessions.
Exit criteria appear in your plan and include stable symptom scores, consistent coping skills use, and a relapse-prevention strategy.\ Tides Mental Health offers continued care options and can arrange follow-up or stepped-down services when you’re ready.
Integration with Other Levels of Care
IOP fits between full-time programs and weekly therapy.\ It provides structured group and individual sessions while keeping you in daily life.
You can use IOP for stepping down after inpatient care or stepping up when weekly therapy isn’t enough.
Continuum of Care Overview
The continuum links detox, inpatient, partial hospitalization (PHP), intensive outpatient (IOP), and standard outpatient care.\ IOP typically offers 9–20 hours per week of therapy, skills training, and case management.
This level suits adults working or studying who need more than weekly counseling for anxiety, depression, life transitions, or relationship issues.\ Tides Mental Health offers IOPs that combine group CBT, individual sessions, and family or couples counseling.
About 60–70% of sessions are virtual, with 30–40% in-person in the Chicago area.\ You’ll get a personalized plan that sets goals, tracks progress, and coordinates with medical or residential teams when needed.
Transitioning to and from IOPs
Entering IOP usually follows a clinical assessment that matches your needs to intensity and services.\ If you come from inpatient or PHP, your care team will create a step-down plan: medication management, relapse prevention, and scheduled therapy hours to keep momentum.
If you step up from weekly outpatient care, IOP adds structure with more frequent groups and focused skill practice.\ When leaving IOP, the plan moves you to standard outpatient therapy, continued virtual check-ins, or community supports.
Tides Mental Health coordinates referrals, documents progress, and offers ongoing virtual follow-up to prevent gaps.\ You retain access to couples or family sessions as needed to support real-life changes.
Unique Considerations and Variations
Programs change by population needs and delivery method.\ You’ll see tailored groups, different session lengths, and a mix of virtual and in-person options that affect scheduling, privacy, and family involvement.
Specialized IOP Populations
IOPs often group participants by specific needs to speed progress and keep sessions relevant.
You may find tracks for adults managing anxiety, depression, life transitions, or relationship issues.
These tracks use targeted therapies like CBT for anxiety and depression.
Couples and family sessions are offered for relationship work, and skills training is provided for life changes.
If you need care for a child or teen, ask about expanding services.
Tides Mental Health offers adult-focused care now and plans to add child and adolescent programs.
This allows you to choose a provider that will support your family as needs grow.
Group sizes, session frequency, and clinician expertise matter.
You should confirm clinicians’ training in your concern and whether family members join sessions.
In-person options are available in the Chicago area if you prefer face-to-face care.
Telehealth and Remote IOP Options
Telehealth IOPs give you flexibility when you juggle work, school, or family.
Most programs run 60–70% virtually, with 30–40% in person, so you can keep daily responsibilities while staying in treatment.
Virtual sessions include live group therapy, individual counseling, and family check-ins.
Expect secure video platforms, digital worksheets, and clear rules about privacy and attendance.
Ask how the program handles crises remotely and what local emergency steps they provide.
If you prefer some in-person contact, you can blend formats.
Tides Mental Health supports a hybrid model: virtual care for routine work and Chicago-based sessions when hands-on evaluation or family meetings help your progress.
Outcomes and Program Evaluation
You will learn how programs track clinical change and how follow-up checks keep care aligned with your goals.
The focus is on measurable progress, symptom change, functional gains, and continued supports after discharge.
Measuring Success in IOPs
You track progress with standard symptom scales, attendance, and behavior measures.
Common tools include PHQ-9 for depression and GAD-7 for anxiety; these give numbers you and clinicians can compare over time.
Clinicians also record session attendance, homework completion, and relapse or crisis events to assess engagement and risk.
Program-level metrics matter too.
Look for reports of reduced symptom scores, improved work or relationship functioning, and drop in emergency visits.
Data should guide weekly care-plan changes and decisions about stepping down to less intensive care.
Long-Term Follow-Up
Long-term checks confirm whether gains last and whether new supports are needed. Typical follow-up points occur at 30, 90, and 180 days after discharge.
Providers collect symptom scales, substance use reports if relevant, and information on employment, school, or family functioning. Care teams use follow-up to adjust outpatient therapy or reconnect you to IOP if relapse risk rises.
Family or couples outcomes receive targeted review when those areas were treatment goals. Tides Mental Health offers scheduled virtual follow-ups and in-person options in Chicago to monitor your progress and arrange continued counseling or referrals as needed.